Introduction [last update: March 2023]
We know how complex this rapidly developing area is. You may find some answers below, but please contact us if you have specific questions or concerns and we will do our best to answer them or forward your enquiry to relevant partners. You might also want to follow our YouTube playlist on social prescribing and integrated care systems.
The government's position on social prescribing
Social Prescribing is currently being championed by both the Department of Health and NHS England in its Long-Term Plan. The Secretary of State for Health and Social Care, Matt Hancock, spoke about culture and creativity in relation to social prescribing in November 2018 at the King’s Fund. He said
The arts can help keep us well, aid our recovery and support longer lives better lived.
And
And I want to say this very frankly, social prescribing reduces the over subscription of drugs. It can lead to the same or better outcomes for patients without so many pills and it saves money for the NHS because many of these social cures are either free or cheaper.
While many of us have long campaigned for the demedicalisation of care and support the basic aims of social prescribing, there remain concerns about funding for community (VCSE) providers. The Secretary of State for Health & Social Care has worried the sector in the past (see his own video from the launch of the NASP) by referring to provision as cheap by comparison to medical interventions, or even free. He has more recently said, however, that as with pharmaceutical products, funding should follow the patient need to the intervention delivered. (Unfortunately no transcript was made of this speech at the Southbank Centre in early 2020.)
More organisations are articulating the need to support the delivery organisations actually providing the 'prescriptions': A Feb 2020 report from the National Lottery Community Fund, for example, says
It’s essential that the services and activities recommended to patients are also adequately and sustainably funded.
The September 2020 National Voices report Rolling Out Social Prescribing articulates the importance of improving linkworkers' roles and management, and also supporting the infrastructure of voluntary and community sector so that it can meet the health sector on equal terms:
Some concerns relate directly to the current NHS rollout and recruitment of link workers:
- The funding and management arrangements, role descriptions and performance expectations that are being put in place for new link workers
- The measures being used to assess the outcomes of social prescribing
Respondents also raised structural issues underpinning successful social prescribing:
- The need for funding to help the VCSE sector meet increased demand
- The need to ensure that social prescribing actively tackles inequality
- The need to invest in relationships and support ongoing collaboration and partnership (p.6)
Government funding
In August 2018 the government announced funding for 23 pilot schemes across the country, to a total of £4.5m. Some cultural work was included in this phase but to the best of our knowledge this represents a relatively small proportion of the social prescribing activities funded. You can read about the schemes here.
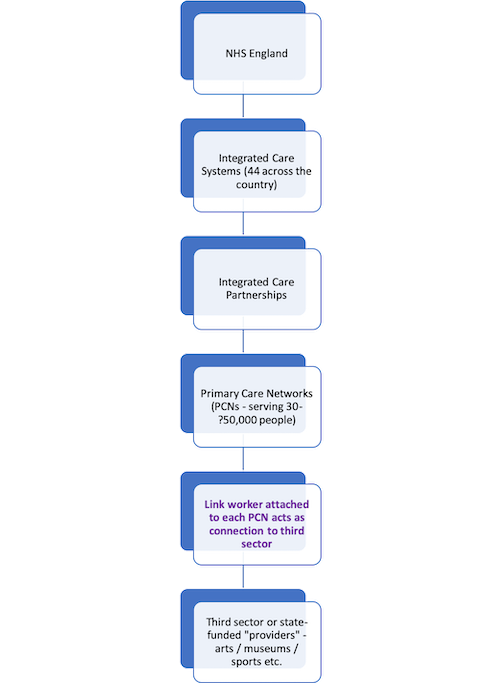
Further funding was announced to support 1,000 link workers (see below) in January 2019. The NHS Long Term Plan says that
Over 1,000 trained social prescribing link workers will be in place by the end of 2020/21 rising further by 2023/24, with the aim that over 900,000 people are able to be referred to social prescribing schemes by then.
It now seems likely that NHS England is aiming to employ roughly 4,500 link workers in the medium term, although as far as we know there has been no official announcement of this larger number.
National funding for ‘providers’ (i.e. organisations or individuals providing the activities) is so far limited to the Thriving Communities Fund detailed above. In some areas Clinical Commissioning Groups (CCGs) provide funding for work through their own budgets. In other areas, organisations have funded this work through arts/cultural funding. You can read more about how the sector is funded from our May 2020 survey.
The National Academy for Social Prescribing is being funded to the tune of £5m including some support from Arts Council England.